In the realm of ear health, Fungal Ear Infections stand as a distinctive challenge, often demanding a nuanced understanding for effective management. This article delves into the depths of fungal ear infections, elucidating their causes, symptoms, and the intricacies of their treatment.
Unraveling the Basics
Fungal Ear Infection Defined:
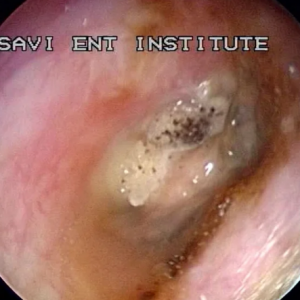
A fungal ear infection, also known as otomycosis, transpires when fungal organisms infiltrate the external auditory canal, causing inflammation and discomfort. Unlike bacterial infections, fungal ear infections are predominantly provoked by molds or yeast, notably the Candida species or Aspergillus.
Causes and Predisposing Factors:
Several elements contribute to the development of Fungal Ear Infections. Prolonged moisture in the ear, compromised immune function, or pre-existing skin conditions can create an environment conducive to fungal growth. Activities such as swimming, using hearing aids, or excessive ear cleaning can exacerbate the risk.
Identifying the Culprits: Symptoms
Fungal Ear Infections manifest with a spectrum of symptoms, often posing a diagnostic challenge. These may include:
Itching (Pruritus): A persistent and bothersome itch within the ear canal.
Pain and Discomfort: Earache, exacerbated by jaw movement or manipulation of the ear.
Discharge: Often presenting as a foul-smelling, yellowish discharge.
Hearing Impairment: Partial loss of hearing, especially if the infection progresses.
Navigating the Diagnostic Landscape
Accurate diagnosis of fungal ear infections requires a meticulous examination by a healthcare professional. This may involve a visual inspection of the ear canal using an otoscope and, in certain cases, a sample collection for laboratory analysis.
Tailoring Treatment Approaches
Topical Antifungal Medications:
The cornerstone of Fungal Ear Infection treatment lies in the application of topical antifungal agents. These medications, often in the form of eardrops, target the specific fungi causing the infection. Common antifungals include clotrimazole, miconazole, or acetic acid solutions.
Addressing Underlying Factors:
In tandem with antifungal therapy, addressing underlying factors is pivotal. Mitigating excessive moisture, managing skin conditions, and adopting meticulous ear hygiene contribute significantly to the treatment’s efficacy.
Oral Antifungal Medications:
In cases of severe or persistent infections, oral antifungal medications may be prescribed. These systemic treatments are reserved for instances where topical agents alone prove insufficient.
Proactive Prevention Strategies
Preventing the recurrence of fungal ear infections involves a multifaceted approach:
Ear Protection: Use earplugs while swimming to prevent water retention.
Avoid Q-Tips: Refrain from inserting cotton swabs or other objects into the ear canal, minimizing the risk of skin damage.
Maintain Dry Ears: Thoroughly dry ears after exposure to moisture, ensuring an unfavorable environment for fungal growth.
Seeking Professional Guidance
Prompt consultation with a healthcare professional is imperative if fungal ear infection symptoms arise. Self-diagnosis and treatment attempts may exacerbate the condition, underscoring the importance of expert intervention.
In Conclusion
In the symphony of ear health, understanding the nuances of fungal ear infections is paramount. From their subtle origins to the complexities of treatment, this exploration aims to empower individuals with insights to navigate the challenges posed by these distinctive infections. As with any medical condition, seeking professional advice ensures a harmonious journey towards optimal ear health.